
For rapid recovery, compression boots are demonstrably superior to massage for lactate clearance due to their systemic effect on venous return.
- Intermittent Pneumatic Compression (IPC) mimics the body’s natural muscle pump, moving metabolic waste centrally.
- Massage guns excel at localized, targeted benefits like pre-workout neural activation and breaking up specific adhesions.
Recommendation: Prioritize compression boots for post-exertion flushing and use a massage gun for targeted pre-activation or specific stiff muscle groups, but not as your primary lactate clearance tool.
For a tournament athlete with less than 24 hours to recover, every decision counts. The burning in your legs isn’t just fatigue; it’s a physiological signal of metabolic byproducts like lactate demanding clearance. The market is flooded with advanced recovery tools, but the common advice to simply “use a recovery tool” is dangerously vague. Many athletes grab a massage gun or pull on compression boots without understanding the fundamental difference in their mechanisms, potentially choosing a suboptimal tool for their most pressing need.
The debate often centers on which device “feels” better, but for an elite performer, the only metric that matters is physiological effect. We look at a massage gun as a tool for targeted relief and boots as a systemic circulatory aid. This perspective is a start, but it misses the crucial element of timing and mechanism. Does a massage gun’s percussive force actually move blood lactate, or does it just distract the nervous system from pain? Do compression boots risk blunting the inflammatory signals necessary for muscle adaptation?
The true key to accelerated recovery isn’t choosing one superior tool, but mastering physiological sequencing. This analysis moves beyond a simple “boots vs. massage” comparison. Instead, we will dissect the specific, data-backed mechanisms of each modality—from external pressure and percussive therapy to thermal stress and sensory deprivation. The goal is to build an evidence-based decision framework, allowing you to deploy the right tool at the right time to clear lactate, manage inflammation, and prime your system for the next round of competition.
This article provides a detailed breakdown of the physiological impact of various advanced recovery modalities. By understanding how each tool works at a systemic and cellular level, you can construct a recovery protocol that is both efficient and effective for high-stakes competition.
Summary: A Mechanistic Guide to Advanced Athlete Recovery
- How external pressure aids venous return when your legs are dead?
- When to use a massage gun: Pre-workout activation or post-workout relaxation?
- Active Recovery or Passive Rest: Does EMS actually move blood while you sit on the couch?
- The inflammation error that blunts your muscle growth signal
- How floating reduces cortisol and muscle tension simultaneously?
- When to schedule a deep-tissue massage relative to your race day?
- Cryotherapy or Sauna: Which triggers better hormonal adaptation after endurance?
- Hot vs. Cold: Which Spa Cycle Accelerates Recovery After a Marathon?
How external pressure aids venous return when your legs are dead?
When your legs feel heavy and unresponsive, the underlying issue is often inefficient venous return. After intense exercise, metabolic byproducts, including lactate, pool in the extremities. The body’s natural “muscle pump” mechanism, where muscle contractions squeeze veins to push deoxygenated blood back to the heart, becomes overwhelmed. This is where external pressure, specifically Intermittent Pneumatic Compression (IPC) from devices like recovery boots, offers a powerful solution. By creating a gradient of pressure that moves sequentially up the limb, these boots mechanically mimic and amplify the muscle pump.
This mechanism isn’t just theoretical; it has a direct and measurable impact on lactate clearance. While passive rest relies on the body’s slow, unaided circulatory processes, recent controlled trials demonstrate that intermittent pneumatic compression results in a 15% faster lactate clearance compared to passive rest. Some systems are even more effective; further peer-reviewed studies on leading compression systems demonstrate an 80% lactate clearance improvement versus passive recovery. This is a significant advantage when the recovery window is short.
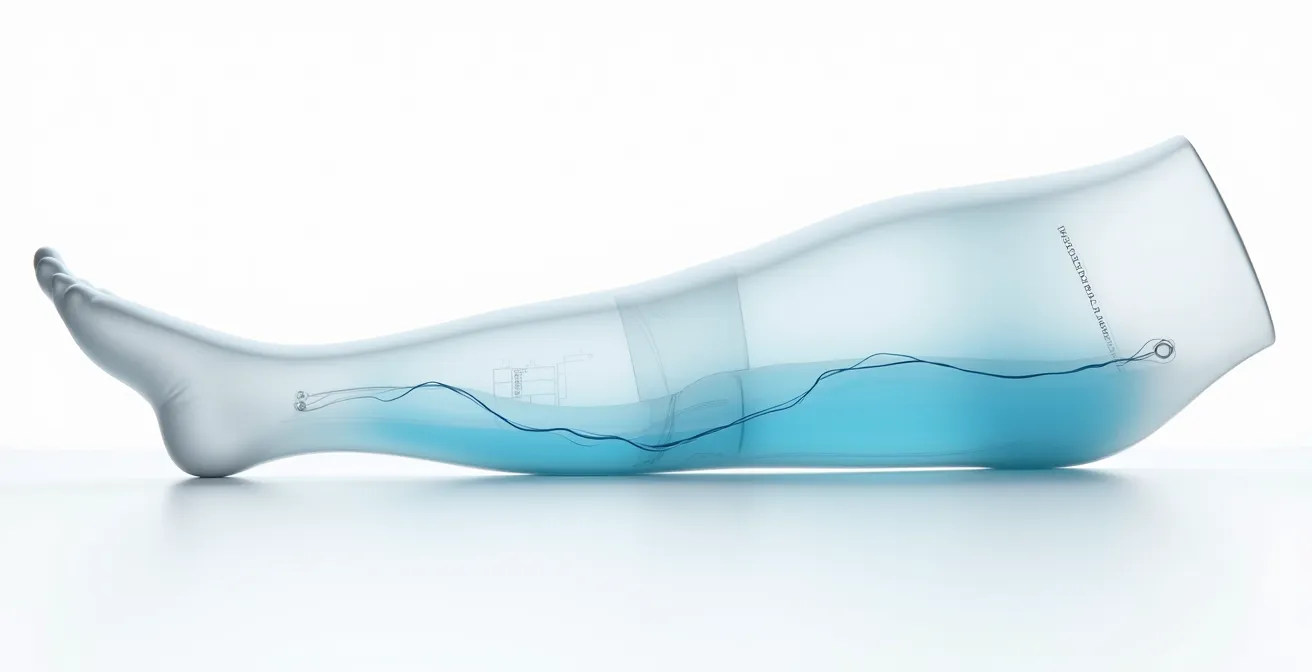
The visualization above shows how the chambers inflate in sequence, creating a “milking” action that forces stagnant fluid from the ankle towards the thigh and into central circulation. For an athlete, a typical effective session lasts between 20 to 60 minutes at a medium to high intensity. The primary disadvantage can be the cost and lack of portability, but for purely systemic flushing of metabolic waste, its mechanistic superiority is clear. It provides a systemic solution for a systemic problem.
When to use a massage gun: Pre-workout activation or post-workout relaxation?
Unlike the systemic flushing action of compression boots, a massage gun—or percussive therapy device—delivers a localized effect. Its power lies in using rapid, concentrated pulses to manipulate soft tissue, making its application highly dependent on the desired outcome: neural activation or muscle relaxation. The choice between using it pre- or post-workout fundamentally alters its purpose and the protocol required.
For pre-workout activation, the goal is to prime the nervous system and increase blood flow to specific muscles. Using a high frequency with low amplitude stimulates mechanoreceptors in the muscle and fascia, essentially “waking up” the muscle-brain connection. This isn’t just a feeling; NIH studies have shown that percussive therapy can lead to an 18% improvement in range of motion when used as part of a warm-up. This makes it an excellent tool for preparing for explosive movements or overcoming feelings of localized tightness before competition.
Conversely, for post-workout relaxation, the protocol shifts. Here, the aim is to decrease muscle tone and reduce perceived stiffness. This requires a lower frequency and higher amplitude to penetrate deeper into the muscle belly. This application can help alleviate adhesions and improve fluid dynamics in a targeted area. While daily use is generally safe for short durations, it’s crucial to avoid using it on bony prominences, nerves, or acutely injured areas. The key is to see the massage gun not as a primary lactate clearance tool, but as a precision instrument for managing tissue quality and neural state.
Your Action Plan: Evidence-Based Massage Gun Protocols
- Neural Priming (Pre-Workout): Use a high frequency/low amplitude setting for 30 seconds per muscle group to activate mechanoreceptors. Apply 5-10 minutes before training to optimize range of motion.
- Muscle Relaxation (Post-Workout): Use a low frequency/high amplitude setting for up to 90 seconds per muscle to address stiffness. This can help reduce perceived soreness.
- Adaptation Window: To avoid blunting strength adaptation signals, wait at least 2 hours after a heavy resistance training session before performing deep percussive therapy on the worked muscles.
- Nervous System Regulation: Enhance the relaxation effect by pairing a 10-minute post-workout session with controlled breathing techniques, such as physiological sighs, to improve Heart Rate Variability (HRV).
- Targeted Application: Focus only on the muscle belly. Avoid joints, bony areas, and the front of the neck or spine to prevent injury or nerve irritation.
Active Recovery or Passive Rest: Does EMS actually move blood while you sit on the couch?
The concept of “active recovery” is praised for its ability to clear metabolic byproducts more effectively than complete rest. However, for a physically exhausted athlete, even a light spin on a bike can be too demanding. Electrical Muscle Stimulation (EMS) presents a compelling hybrid: a passive modality that induces the physiological effects of active recovery. By sending electrical impulses through electrodes placed on the skin, EMS causes involuntary muscle contractions, effectively creating a “muscle pump” without any cardiovascular load or conscious effort.
This isn’t a placebo effect; EMS generates tangible physiological changes. It directly forces the muscles to contract and relax, pushing blood and lymphatic fluid through their respective vessels. This effect isn’t just localized to the limbs. Remarkably, research published in BMC Neuroscience found that electrical muscle stimulation applied to the legs significantly increased cerebral blood flow, with internal carotid artery blood flow rising from 330 to 371 mL/min. This indicates a systemic circulatory benefit, helping to deliver oxygen and clear waste not just from the muscles, but throughout the body, including the brain.

While compression boots provide external pressure, EMS creates internal pressure via muscle contraction. It’s a way to “earn” the benefits of active recovery while in a state of complete passive rest. For the tournament athlete sitting on a bus or in a hotel room, this is a game-changer. It allows the body to engage its waste-clearance mechanisms without expending precious energy, making it a highly efficient tool for recovery in constrained environments. The key is to use programs designed for recovery (low frequency, often called “active recovery” or “massage” modes) rather than strength-building protocols.
The inflammation error that blunts your muscle growth signal
In the quest for rapid recovery, athletes often adopt a “more is better” approach to fighting inflammation. While excessive, chronic inflammation is detrimental, the acute inflammatory response following exercise is a critical signaling process for muscle repair and adaptation. Aggressively blunting this signal with improperly timed interventions can paradoxically hinder recovery and long-term gains. This is the “inflammation error”: treating a necessary biological process as a problem to be eradicated entirely.
Recovery modalities like compression boots are often marketed as tools to reduce muscle damage and soreness. However, the data on their direct impact on muscle damage markers is nuanced. As noted in the Journal of Physiotherapy Systematic Review:
IPC has long been established in medical contexts to improve venous return and prevent thrombosis, but its effects on exercise-induced muscle damage markers are inconsistent.
– Journal of Physiotherapy Systematic Review, Hyperice Australia Recovery Insights 2025
This is supported by biomarker analysis. For instance, research examining muscle damage biomarkers reveals that Creatine Kinase (CK) levels show no significant difference between groups using IPC and control groups. This suggests that the primary benefit of compression boots is circulatory enhancement and fluid management, not a direct reduction in cellular muscle damage. Their value lies in clearing metabolic waste that *contributes* to soreness, rather than stopping the essential inflammatory repair process itself. The mistake is not using the tool, but using it with the wrong expectation—expecting it to erase damage when its real strength is optimizing the environment for repair.
How floating reduces cortisol and muscle tension simultaneously?
While mechanical tools target the musculoskeletal system, flotation-REST (Restricted Environmental Stimulation Therapy) addresses recovery from a neuropsychological angle. Floating involves lying effortlessly in a dark, soundproof tank filled with a supersaturated solution of Epsom salt and water heated to skin temperature. This unique environment tackles two key barriers to recovery simultaneously: elevated cortisol and persistent muscle tension.
The primary mechanism for cortisol reduction is the profound sensory restriction. By removing external stimuli—sight, sound, touch, and even gravity’s full effect—the central nervous system’s load is drastically reduced. This down-regulates the hypothalamic-pituitary-adrenal (HPA) axis, the body’s primary stress response system. With the “fight or flight” signals muted, production of the stress hormone cortisol decreases significantly, shifting the body into a parasympathetic “rest and digest” state that is optimal for cellular repair and mental restoration.
Simultaneously, the therapy targets muscle tension. The extreme buoyancy created by over a thousand pounds of dissolved Epsom salt (magnesium sulfate) allows the body to de-load completely. Every muscle, tendon, and joint is relieved from the constant work of fighting gravity. This physical release is complemented by the theoretical benefit of transdermal magnesium absorption. Magnesium is a crucial mineral for muscle relaxation, acting as a natural calcium blocker to help muscle cells relax after contracting. While the extent of absorption through the skin is debated, the combination of profound physical unloading and a magnesium-rich environment provides a powerful stimulus for reducing neuromuscular tension, allowing muscles to reset their baseline tone.
When to schedule a deep-tissue massage relative to your race day?
A deep-tissue massage is a powerful but invasive recovery tool. It creates micro-trauma in the muscles to break down adhesions and restore tissue quality. While beneficial in a training block, its timing relative to a major competition is critical. Scheduling it too close to race day can leave an athlete feeling sore, tired, and physiologically compromised rather than primed for performance. The key is to periodize massage just like training.
The final, intensive deep-tissue session should be scheduled well in advance of the event. This allows the body sufficient time to resolve the inflammation induced by the massage and complete the repair process, leaving the tissue healthier and more pliable. As the race approaches, the intensity of any manual therapy must decrease dramatically. The days immediately preceding the event are a “no-go zone” for any aggressive bodywork. The focus should shift from tissue remodeling to light, circulatory flushing to keep muscles loose without inducing further stress.
A structured timing protocol is essential for maximizing benefits and minimizing risk:
- Final Deep-Tissue Session: Schedule this no later than 5-7 days before race day. This provides a buffer for any residual soreness and inflammation to fully clear.
- The “No-Go Zone”: Avoid all deep-tissue work within the 3-4 days leading up to the competition. The risk of negative impact far outweighs any potential benefit.
- Pre-Race Flush: If a massage is desired 1-2 days before the race, it must be a light, circulatory “flush” massage only. The goal is to promote blood flow and relaxation, not to work out deep knots.
- Post-Race Recovery: Wait at least 24-72 hours after the race before getting any deep-tissue work done. The appropriate waiting period depends on the level of muscle soreness and damage incurred during the event. Immediately post-race, non-invasive modalities like compression boots are a safer choice for managing inflammation.
Key Takeaways
- Mechanism is King: The most effective recovery strategy is built on understanding *how* a tool works, not just what it does. Compression boots for systemic flushing, massage guns for local targeting.
- Timing Determines Outcome: A modality’s effect is context-dependent. Percussive therapy is for pre-workout activation or post-workout relaxation, not both with the same protocol. Deep tissue massage is a pre-taper tool, not a pre-race one.
- Don’t Blunt the Signal: Acute inflammation is a necessary part of adaptation. The goal of recovery tools is to manage the environment (clear waste, reduce pain) without shutting down these essential biological repair processes.
Cryotherapy or Sauna: Which triggers better hormonal adaptation after endurance?
Beyond mechanical interventions, thermal stress—deliberately exposing the body to extreme hot or cold—is a potent way to trigger adaptive hormonal responses. For the endurance athlete, the choice between cryotherapy (cold) and sauna (heat) is not about which feels better, but which hormonal cascade best serves their recovery goal. Each modality stimulates a distinct and powerful physiological pathway.
Cryotherapy and cold exposure act as a powerful activator of the sympathetic nervous system. The acute shock of cold triggers a massive release of norepinephrine, a hormone and neurotransmitter that dramatically reduces inflammation system-wide, enhances focus and alertness, and can elevate mood. For an athlete feeling foggy and inflamed after a grueling event, this provides an immediate neurological and anti-inflammatory boost. The cold stimulus also encourages the conversion of energy-storing white adipose tissue into metabolically active brown adipose tissue, a long-term benefit for body composition and thermal regulation.
Sauna and heat exposure, on the other hand, elicit a different set of adaptations. The primary benefit is the robust release of Heat Shock Proteins (HSPs). These proteins act as intracellular chaperones, repairing misfolded proteins damaged by oxidative stress from exercise and protecting cells from future damage. Furthermore, repeated sauna use has been shown to significantly increase the release of Human Growth Hormone (HGH), a key hormone for tissue repair, muscle growth, and overall recovery. The cardiovascular strain from heat also mimics moderate exercise, improving cardiovascular function and plasma volume. The choice is strategic: use cold for acute inflammation control and a neural reset, and use heat for deep cellular repair and a powerful anabolic hormone boost.

Hot vs. Cold: Which Spa Cycle Accelerates Recovery After a Marathon?
After the immense stress of a marathon, the body is in a state of widespread inflammation and muscle damage. The right thermal spa cycle can significantly accelerate recovery, but a misstep can either be ineffective or delay healing. The key is to phase the intervention, matching the thermal stimulus (hot, cold, or contrast) to the body’s physiological state in the hours and days following the race. A one-size-fits-all approach is inefficient; a sequenced protocol is essential.
In the immediate aftermath (Phase 1), the primary goal is to control the massive inflammatory response and mitigate swelling. During this period, cold is the only appropriate choice. In Phase 2, the goal shifts to promoting circulation to bring nutrients to damaged tissues and clear out waste, making contrast therapy ideal. Finally, in Phase 3, the focus turns to increasing tissue mobility and final relaxation, where heat becomes dominant. Compression therapy can be integrated throughout, but is best used after the initial 4-hour window to avoid interfering with the acute inflammatory process while still enhancing circulation.
This phased approach can be structured with specific time frames and goals, as outlined in protocols developed by leading athletic organizations. The following table provides a clear framework for post-marathon thermal recovery.
| Recovery Phase | Time Frame | Primary Modality | Physiological Goal |
|---|---|---|---|
| Phase 1 | 0-24 hours | Cold only (ice bath/cryo) | Control massive inflammation |
| Phase 2 | 24-72 hours | Contrast therapy | Promote blood flow to damaged areas |
| Phase 3 | 72+ hours | Heat dominant (sauna/warm bath) | Increase tissue extensibility |
| Compression Integration | After 4+ hours | 20-30 min sessions | Enhance circulation without inflammation |
As this framework for recovery illustrates, moving from pure cold to contrast and finally to heat respects the body’s natural healing timeline. Cold first contains the “fire” of inflammation, contrast then acts as a vascular pump, and heat helps in the final remodeling of the tissue. This strategic sequencing ensures that each intervention provides the right stimulus at the right time, maximizing recovery speed and effectiveness.
By moving beyond a simplistic “A vs. B” mindset and adopting a nuanced, mechanism-based approach, an athlete can transform recovery from a passive waiting game into an active, strategic advantage. Evaluating and deploying these advanced modalities based on their specific physiological impact is the next frontier in performance optimization.